Silver: A Robust Antimicrobial Agent
Incorporating silver ions into the CSpring MK3® benefits users from a heightened level of protection against microbial contamination. This addition ensures that the water chamber remains not only consistently replenished but also continuously sanitized. Silver ions work by binding to bacterial cell walls, blocking the transport of substances in and out of the cells, and penetrating the cells to disrupt key cellular functions such as DNA replication and energy production.
The integration of silver ion technology in the CSpring MK3 aims to provide users with peace of mind regarding the cleanliness of their CPAP system, reducing the risk of respiratory infections and enhancing overall therapy effectiveness. This innovative approach underlines our commitment to advancing CPAP technology by leveraging the antimicrobial prowess of silver, thus ensuring that each breath taken is not just moist and comfortable but also clean and safe.
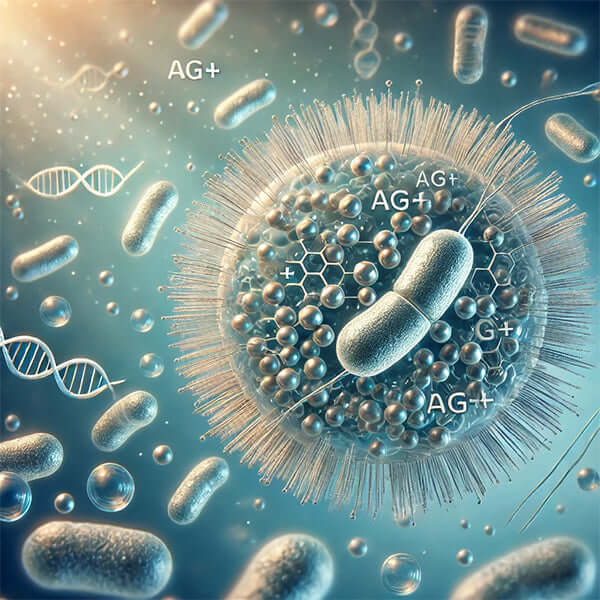
Silver is renowned for its potent antimicrobial properties, effectively eliminating bacteria, fungi, and certain viruses. The secret to its effectiveness lies in the positively charged silver ions (Ag+), which are known to disrupt multiple biological processes in microorganisms.
How Silver Ions Combat Microbial Growth
Silver ions integrate into bacterial cell membranes and attach to proteins that control the transport of substances into and out of cells. These ions also penetrate the cells, where they interfere with DNA replication and halt cell division. Moreover, silver disrupts the bacterial respiratory system, crippling the cell's energy production. Eventually, this leads to the rupture of the cell membrane and the destruction of the bacteria.
Silver's historical use in wound care underscores its safety and efficacy. Modern silver-containing dressings are particularly noted for their excellent safety profile. The body naturally eliminates excess silver through processes like epidermal turnover and metal detoxification pathways in the liver and kidneys, resulting in excretion via feces and urine. Although some silver may remain in the body, it typically forms highly stable, non-bioavailable complexes, contributing to its safety.
Antimicrobial Resistance and Silver
The potential for bacteria to develop resistance to silver has been a point of discussion, especially with the rising concern over antibiotic resistance. However, silver's multiple mechanisms of antimicrobial action make it less likely to provoke resistance compared to antibiotics. While laboratory studies suggest the possibility of resistance, clinical evidence does not currently indicate a significant threat, allowing silver-containing dressings to remain vital in managing wound infections.
* image depicting the effects of silver ions on a bacterial cell, with detailed visualizations of their interactions with the cell membrane, membrane proteins, and DNA. This image emphasizes the mechanism of action, showing how the ions disrupt cell functions and lead to the cell's deterioration.

References and article links:
Peer-reviewed medical journal reference










Leave a comment: